Background: Liso-cel is an autologous, CD19-directed, 4-1BB CAR T cell product administered at equal target doses of CD8 + and CD4 + CAR + T cells that has demonstrated efficacy and favorable safety based on clinical studies. Liso-cel is approved in the US for the treatment of adults with R/R LBCL after 1 or more lines of systemic therapy, but data describing outcomes in patients treated with liso-cel in the real-world setting are limited. We report real-world clinical effectiveness and safety of commercial liso-cel in patients with R/R LBCL based on a postmarketing study using data collected at the Center for International Blood and Marrow Transplant Research (CIBMTR).
Methods: This is a noninterventional, observational, multicenter study of US patients who were followed in the CIBMTR Cellular Therapy Registry between February 2021 and November 2022 after infusion with commercial liso-cel (conforming product only) for the treatment of R/R LBCL. Patients who received nonconforming product are being followed in a separate postmarketing study. The primary objective was to evaluate the real-world clinical effectiveness and safety outcomes of patients with R/R LBCL receiving liso-cel, including ORR, CR, duration of response (DOR), progression-free survival (PFS), overall survival (OS), and risk of cytokine release syndrome (CRS) and immune effector cell-associated neurotoxicity syndrome (ICANS). Results were analyzed and reported descriptively.
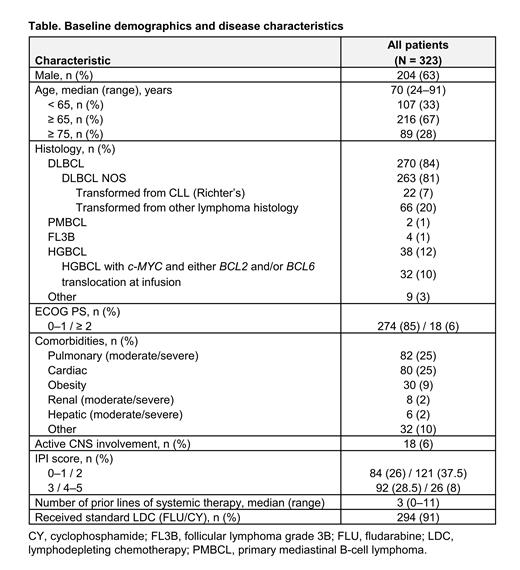
Results: At data cutoff (May 4, 2023), 323 patients who received commercial liso-cel across > 50 treatment sites were included in the analysis. The median vein-to-vein time (from leukapheresis to liso-cel infusion) was 36 days (IQR, 34‒42), which is consistent with clinical studies of liso-cel. The median age was 70 years (range, 24‒91). Patients included those with high-risk disease (Table). Most patients had DLBCL not otherwise specified (NOS; 81%), 27% had disease transformed from indolent lymphoma, 12% had high-grade B-cell lymphoma (HGBCL), 37% had International Prognostic Index (IPI) ≥ 3, 6% had active CNS involvement, and 15% had prior transplant. The median number of prior lines of systemic therapy was 3 (range, 0‒11), with 25% of patients having received ≥ 4 lines. The median time from diagnosis to liso-cel infusion was 1.4 years (range, 0.2‒29.7). At a median follow-up of 7.4 months, ORR was 79%, with a 65% CR rate. Median time to response was 1.2 months (IQR, 1.0‒3.1). The median DOR has not been reached; DOR rate at 6 months was 73% (95% CI, 66%‒79%). The median PFS and median OS had not been reached at the time of data cutoff. Estimated 6-month PFS and OS rates were 64% and 82%, respectively. Most events of CRS and ICANS were of low grade, with no CRS and ICANS reported in 48% and 70% of patients, respectively. Overall, 52% of patients had CRS and 3% had grade ≥ 3 events. There was a high concordance on CRS grading per Lee 2014 and American Society for Transplantation and Cellular Therapy criteria. The most common treatments for CRS were tocilizumab (20%) and corticosteroids/tocilizumab (12%). ICANS was seen in 30% of patients, with grade ≥ 3 events in 11%. ICANS was mostly treated with corticosteroids (12%) and corticosteroids/antiepileptics (5%). Based on the attributed cause of death, grade 5 CRS or ICANS were observed in 3 and 3 patients, respectively, and all but 2 patients had concomitant causes of death, including disease progression (n = 3) and hemophagocytic lymphohistiocytosis (n = 2). Prolonged cytopenia (grade 4 thrombocytopenia and/or neutropenia persistent at 30 days postinfusion) occurred in 10% of patients.
Conclusions: This is the first large, multicenter, real-world study of patients with R/R LBCL who received commercial liso-cel in the US. Baseline characteristics of patients treated in the real-world setting were consistent with or worse than the liso-cel registrational study experience, including the percentage of patients who had received ≥ 4 lines of prior systemic therapy (25% vs 26% in TRANSCEND). One-time infusion of liso-cel demonstrated deep and durable responses in patients with R/R LBCL across a broad age range, including those with high-risk features characteristic of poor prognosis. The incidence of severe (grade ≥ 3) CRS and ICANS was low. These results further support liso-cel as a therapeutic option with a favorable benefit/risk profile for a broad, real-world population of patients with R/R LBCL.
Disclosures
Crombie:ADC Therapeutics: Consultancy; Karyopharm: Consultancy; Seagen: Consultancy; Genmab: Consultancy; Dana-Farber Cancer Institute: Current Employment; Kite Pharma: Consultancy; Bayer: Research Funding; Abbvie: Research Funding; Merck: Research Funding; Genetech/Roche: Research Funding; MorphoSys/Incyte: Consultancy. Nastoupil:AstraZeneca: Honoraria; Gilead Sciences/Kite Pharma: Honoraria, Research Funding; Regeneron: Honoraria; Genentech, Inc., Genmab, Gilead/Kite, Janssen, Merck, Novartis, Takeda: Honoraria, Research Funding; Daiichi Sankyo: Honoraria, Research Funding; DeNovo: Honoraria; Caribou Biosciences: Honoraria, Research Funding; Bristol Myers Squibb/Celgene: Honoraria, Research Funding; ADC Therapeutics: Honoraria; AbbVie: Honoraria. Andreadis:Kite/Gilead: Consultancy; BMS: Consultancy, Other: Grants or contracts ; Novartis: Consultancy, Other: Grants or contracts ; Genentech: Other: Grants or contracts ; Merck & Co., Inc.: Research Funding. Isufi:Incyte: Consultancy; Abbvie: Consultancy; Genmab: Consultancy; Gilead: Consultancy, Current equity holder in publicly-traded company; ADC Therapeutics: Consultancy; Beam Therpauetics: Consultancy. Hunter:Novartis: Consultancy, Honoraria; Bristol Myers Squibb: Consultancy, Honoraria; Kite Pharma: Consultancy, Honoraria, Speakers Bureau; Genmab: Consultancy, Honoraria, Speakers Bureau; Janssen: Consultancy, Honoraria; ADC Therapeutics: Consultancy, Honoraria; Notable Labs: Consultancy, Honoraria; AbbVie: Consultancy, Honoraria, Speakers Bureau; Genentech: Consultancy, Honoraria; Astellas: Consultancy, Honoraria. Winter:AstraZeneca: Consultancy; Janssen: Consultancy; Seattle Genetics: Consultancy; ADC Therapeutics: Consultancy; BeiGene: Consultancy. Hess:ADC Therapeutics: Consultancy; Bristol Myers Squibb: Consultancy. Barta:Daiichi Sankyo: Consultancy; Affimed: Consultancy; Janssen: Consultancy; Acrotech: Consultancy. Frigault:Kite, BMS, Novartis, Iovance: Consultancy; Kite, Arcellx, Novartis: Research Funding. Palomba:BMS: Honoraria; Cellectar: Honoraria; Kite: Honoraria; Ceramedix: Honoraria; GarudaTherapeutics: Honoraria; Juno: Honoraria, Patents & Royalties; MustangBio: Honoraria; Novartis: Honoraria; Pluto Immunotherapeutics: Honoraria; Rheos: Honoraria; Seres Therapeutics: Honoraria, Patents & Royalties; Smart Immune: Honoraria; Thymofox: Honoraria; Synthekine: Honoraria. Grover:Kite: Honoraria; Genentech: Honoraria; Seagen: Honoraria; Caribou Biosciences: Honoraria; Tessa Therapeutics: Research Funding; Novartis: Honoraria; Sangamo: Current holder of stock options in a privately-held company; Seattle Genetics: Consultancy; ADC Therapeutics: Consultancy, Honoraria. Jain:Incyte: Research Funding; Loxo@Lilly: Research Funding; Myeloid Therapeutics: Consultancy, Honoraria; Kite/Gilead: Consultancy, Honoraria, Research Funding. Moyo:Kite Pharmaceuticals: Consultancy. Patel:Sanofi: Speakers Bureau; CTi BioPharma: Consultancy; orca bio: Research Funding; Kite Pharma: Speakers Bureau. Pophali:SeaGen: Honoraria. Bernasconi:Bristol Myers Squibb: Current Employment, Current equity holder in publicly-traded company. Kitali:Bristol Myers Squibb: Current Employment, Current equity holder in publicly-traded company. Liu:Bristol Myers Squibb: Current Employment, Current equity holder in publicly-traded company. Gharibo:Bristol Myers Squibb: Current Employment, Current equity holder in publicly-traded company. Pasquini:Janssen: Research Funding; Novartis: Research Funding; Kite, a Gilead Company: Honoraria, Research Funding; Bristol Myers Squibb: Consultancy, Research Funding; Kite Brazil: Honoraria.